In September 2012, the 17th Annual CyberPsychology & CyberTherapy Conference (CYBER17) was held. With some of the restrictions to growth acknowledged as early as 2000, the International Association of
CyberPsychology, Training, & Rehabilitation (iACToR) community has become acutely aware of the need to transform itself to quicken the pace of progress. Suggestions made around that time period still remain and continued to be amongst the discussions at CYBER17. In 2000 perhaps these difficulties were acceptable; however, with a multitude of technological advancements, and 12 additional years of research funding, these deficiencies need no longer continue. One remaining stumbling block is the lack of interoperability: the applications and software content are available, but the infrastructure is still lacking to allow widespread deployment of these tools.
The need for an overall shift from institutional healthcare settings to everyday environments, and from treatment to a preventive approach based on new personalised healthcare technologies, is widely recognised and made available by the advancement of Information and Communication Technologies (ICT). The Strategic Approach for the EU for 2008-2013 stated that ‘health is the greatest wealth’ and that ‘health is important for the wellbeing of individuals and society, but a healthy population is also a prerequisite for economic productivity and prosperity’. The strategy of European healthcare envisions innovation coupled with new technologies as the solution to these problems.
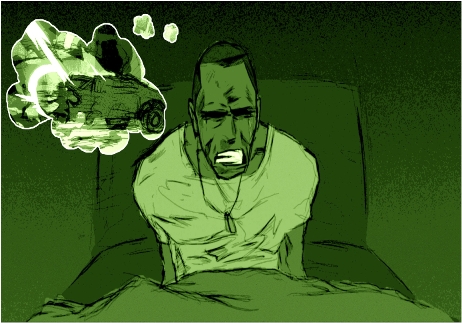
A wide variety of health promotion/disease prevention (wellness) multimedia content has been tested and validated in pilot studies and clinical trials. In addition, virtual reality content for multiple disorders ranging from obesity to posttraumatic stress disorder to cognitive and physical rehabilitation has shown clear efficacy. The development cycle for these technologies involved a migration process beginning with first designing and developing the solutions on desktop platforms, with input from end-users, clinicians and technical design staff. Once pilot studies and randomised, controlled clinical trials were performed, then the technologies were ported to more mobile platforms. Now the challenge is to move from the current mobile devices to a cloud-based solution for even easier access and more widely distributed treatment solutions.
It is critical that a platform now be put in place to deploy these tools for widespread use by stakeholders who may benefit from them; in some cases, these stakeholders will be individual citizens, and in other cases, healthcare providers. In order for this to occur, however, interoperability is essential. An infrastructure must be implemented that will allow applications to work without the necessity of the patient, trainee or clinician/researcher purchasing a separate peripheral device, specific computer or software package to run each app.
As Vice President for the Digital Agenda Neelie Kroes said in a September 2012 interview on the EU Commission’s strategy on cloud computing, good reasons to be in the cloud include interoperability, data portability and reversibility. After the interoperability hurdle has been surmounted by the adoption of cloud computing, the prices of apps can come down as development costs shrink. Secure protocols for transmission of patient data in the cloud are coming online. Therefore, the primary remaining barrier to adoption will be clinician training and patient education, in which the EU has the opportunity to play an important role.